The Treatment of Sleep Apnea in Children
Treatment for sleep apnea in a child will be determined in large part based on the cause and may include allergy treatment, tonsillectomy, and an orthodontic protocol called rapid maxillary expansion. In some children, the use of continuous positive airway pressure (CPAP) machines may be helpful. As children grow closer to adult stature, other treatment options become available.
Continuous Positive Airway Pressure (CPAP)
CPAP treats sleep apnea with air pressure delivered via a mask.
For nearly everyone who has been diagnosed with sleep apnea, the conversation quickly turns to possible treatment options. The most effective and commonly used one is continuous positive airway pressure (CPAP),
but what is CPAP? Take a moment to learn about the basic components of CPAP, including the mask, tubing, and humidifier. Discover how CPAP effectively treats sleep apnea by delivering air pressure via a face mask.
What Is CPAP?
CPAP is the gold standard treatment for obstructive sleep apnea. A CPAP machine provides a constant flow of pressurized air that helps to maintain an open airway by preventing its collapse. This air is delivered via a fitted mask. CPAP has been used to treat sleep apnea since 1981 with Side Effects
Air Leaking From CPAP Masks
By far, an air leak is the most common complaint associated with CPAP use. If the mask does not fit perfectly, air may escape around the edges, especially as you change position while you are sleeping.
Larger masks, such as those that cover the nose and mouth, are more prone to leaks. Leaks may compromise your therapy by reducing the pressure delivered, or they may be noisy and disturb your bed partner.
Air leaks can be reduced by using a nasal mask or nasal pillows. If you are struggling with the fit of your CPAP mask, altering the pressure settings can sometimes be helpful.
If there is too much air pressure, the excessive air escapes around the edges of the mask or out of the mouth. Discuss this with your doctor before changing the settings.
Skin Marks or Rashes
Your CPAP mask may leave marks on your skin if it doesn't fit properly, possibly leading to sores or even ulcers, especially along the bridge of your nose. People with sensitive skin may also develop a rash or skin irritation, especially with masks that contain latex.
Mask liners, barrier creams, loosening the mask, or a better-fitted mask may relieve these symptoms.
Avoiding Marks and Lines From CPAP Mask
Dryness in the Nose or Mouth
Dryness of your nose or mouth often accompanies leakage. This may lead to nosebleeds or may even damage your gums and teeth. If your mouth falls open, air can escape, leading to a parched mouth or tongue.
If your nose is dry, over-the-counter nasal saline spray can help. Using a heated humidifier and heated tubing can also help keep you from drying out. To keep your mouth from falling open, you can try a chinstrap or a full-face mask that covers both the nose and mouth.
Discomfort Breathing Out
Though it is easy to breathe in, you may find it difficult to breathe out against the pressure when you first start using CPAP therapy. This may improve over time, but the effort may also cause insomnia.
In some cases, ramping from a lower initial pressure or a feature to allow easier exhalation can be helpful. It may be necessary to reduce pressures overall. In rare cases, bi-level therapy—in which one pressure is used to breathe in, and a lower pressure is used to breathe out—may be needed.
Air Swallowing
Many people experience air swallowing, called aerophagia (literally "air eating"). If you wake and your stomach is filled with air, this may be due to aerophagia.
Symptoms include:
• Burping
• Farting
• Bloating
Air swallowing can be a sign of CPAP pressures that are too high. Rather than entering your upper airway, the excessive air can enter your stomach via your esophagus.
Reduced pressures may help to prevent this. Other treatments for aerophagia include sleeping wedge pillows, medications used for heartburn and gastroesophageal reflux disease (GERD), and bi-level therapy.
Developing Central Sleep Apnea
After using CPAP therapy, some people may start to experience episodes of the breath-holding characteristic of central sleep apnea. You may have complex sleep apnea if central apneas did not account for the majority of your breathing disturbances before starting CPAP but now contribute to more than five events per hour.
This sometimes resolves in time, and it may be alleviated by simply lowering the CPAP pressure. Sometimes, treatment may require a change to adaptive servo-ventilation (ASV) therapy, in which the volume and speed of air can be set to vary according to your needs.
Face Growth Problems in Children
Children who use CPAP should be monitored to avoid developing growth problems of the mid-face related to the pressure of the mask across the nose. Newer mask styles, including nasal pillows, may reduce this risk.
Claustrophobia
Some people feel confined or enclosed when wearing a mask. This typically resolves over time, particularly if you take the time to adjust gradually to using the mask.
If you have claustrophobia and have trouble wearing your CPAP mask, talk to your doctor about possible treatments for the claustrophobia.
Loud Noise
The noise can interfere with sleep, particularly for the person who you sleep with. While the currently used devices are much quieter than those used in the past, it may take some getting used to. Overall, most partners can adapt more easily to the predictable noise of CPAP than to the noise of snoring, which is very common with obstructive sleep apnea.
Sex Drive
Some people may complain that the use of a CPAP mask is unappealing and could inhibit sex drive for one or both partners. If this is an issue, it is best to have a frank discussion with your partner to decide when you will use it and how to avoid negative feelings about the mask.
Adjusting CPAP Setting
Sometimes, it's necessary to adjust the pressures of the CPAP machine as your risk factors for obstructive sleep apnea change. Several factors can make this necessary, including:
• Weight changes: Excessive weight is a risk for sleep apnea, but if you lose weight you may start to have problems with air swallowing, mask leak, or difficulty breathing out against the pressure. Lowering your CPAP pressure may help.6 Weight gain can also require a change in CPAP pressure.
• Allergies: If you have environmental allergies, optimized treatment with medications or nasal sprays could reduce your pressure requirements by improving airflow through the nasal passage.
• Surgery: Surgical procedures, including tonsillectomy, nasal septoplasty, and soft palate or tongue surgery, may alter your CPAP therapy requirements.
• Substance use: If you smoke, snoring and sleep apnea may become more severe. Alcohol use near bedtime can cause muscle relaxation, worsening your obstructive sleep apnea symptoms. If you discontinue the use of any of these substances, your pressure needs may also be reduced.
• Medications: Medications such as muscle relaxants and benzodiazepines may worsen your symptoms. Discontinuing them may reduce your pressure needs.
Remember that you should have your doctor adjust your settings. It can be dangerous to do it on your own.
Fortunately, changes can often be made to improve the experience with CPAP therapy and to reduce the side effects. If you experience side effects, speak with your sleep specialist or equipment provider, who can suggest solutions for you.
After review of your CPAP data, a determination can be made on how best to change your pressure settings or make other changes.
It is also effective in eliminating snoring, which usually occurs due to the vibration of the tissues in the throat. Although there are many different manufacturers of CPAP equipment, each unit consists of the same basic components.
How a CPAP Machine Works
The CPAP machine is the workhorse of your treatment. With a small motor and fan, it takes in room air, filters it, and generates the air pressure that is the mainstay of treating sleep apnea. Newer units are small, often smaller than a loaf of bread, and relatively quiet. The newest ones make little to no noise. Most run on electricity, but battery units are also available.
The prescribed pressure level is often determined through a sleep study called a polysomnogram. However, it can also be set with an auto titration function (AutoCPAP or APAP) that automatically determines the pressure needed to keep your airway open. The pressure settings are determined by your sleep physician and set by your equipment provider.
In addition to the therapeutic pressure range, there is often a feature that makes it possible to set a pressure ramp. This allows you to fall asleep at a lower pressure that steadily increases to the therapeutic pressure that you need either after a set period of time has elapsed or after your breathing becomes more regular, indicating that you have fallen asleep.
Most models have sophisticated methods of tracking your use with an internal memory card. This data can also be shared via an internal or external modem to cloud-based data storage that can be remotely accessed by your provider. This can help your doctor to assess your compliance with the treatment. It also may determine whether insurance will pay for your continued therapy.
Humidifier
As a comfort measure, it is possible to add humidity to the air that is delivered with an attached humidifier. This is integrated into most newer models. There is a water chamber that generally consists of a plastic reservoir that can be filled with distilled water. Heated humidifiers include a small hot plate that increases the amount of evaporation and moisture put into the inhaled air. As the air passes over the water, direct evaporation occurs and the humidity of the air increases.
It is very important to keep this water reservoir clean, as it can theoretically (and rarely) be a source of recurrent respiratory infection or even mold (however, a study published in 2017 found no increased risk of infections). This will generally only occur if the water is left unattended in the tank for an extended period of disuse.
CPAP Hose or CPAP Tubing
The next component that is standard to all CPAP machines is the CPAP hose or tubing. The CPAP tubing is typically made of a flexible plastic, allowing some degree of movement. Frankly, it resembles the extension hose on a vacuum cleaner. It is typically about 6 feet long. However, with an adapter or connector, it is possible to have two lengths of tubing linked together.
You should be cautious about extending the hose too much as it may decrease the pressure that is ultimately delivered to your face mask. The tubing connects the main output of the machine to the mask. It may be heated and have a temperature setting that you can control to prevent condensation of water into the tubing.
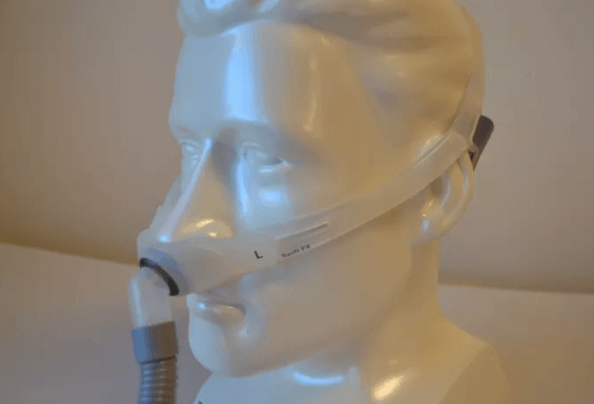
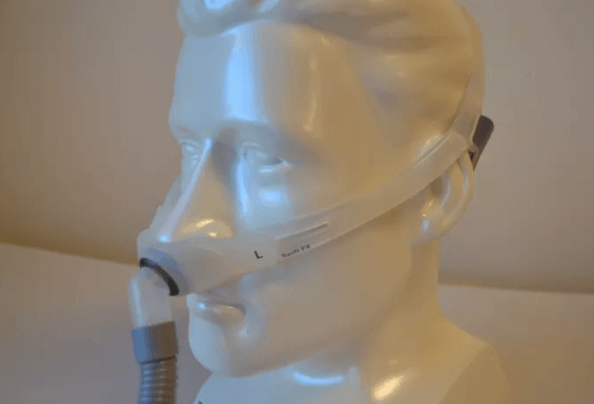
CPAP Mask
The CPAP mask is, undeniably, the most important part of your experience with CPAP. It is where the "rubber meets the road" and it will make you fall in love with your CPAP machine – or hate it. There are three basic styles of CPAP masks:
• Nasal pillows that sit in the nostrils
• Over-the-nose nasal mask
• Full-face mask that covers the nose and mouth
There are dozens of CPAP mask styles available, which makes it all the more important in how to choose one. Work with your physician or equipment provider to find the best mask for you, especially in the first 30 days of CPAP use or any time that you are struggling with leak issues or discomfort from your mask.
4 Steps to Choosing the Right CPAP Mask for Sleep Apnea
1: Choose a CPAP Mask Style That Suits Your Needs
In general, CPAP is meant to provide a constant stream of air that supports your upper airway and keeps it open, thus preventing apnea and snoring. This air may be delivered through your nose, mouth, or both, and the preference may depend on your individual needs.
Most people use a mask that delivers air through their nose. Most nasal masks consist of a triangular-shaped gel or plastic cushion that covers the nose and rests from the bridge of the nose to just below the nostrils. Attached to this will be a headgear, often consisting of fabric, Velcro, or plastic clips that secure the mask to your face. Finally, there will be a plastic hose attaching the mask to the CPAP machine itself.
There are many variations of masks, usually consisting of some combination of ingenuity and marketing. Many masks also have a brace that relieves pressure by adding a few contact points on the forehead. There may be added cushions or seals to prevent marks on your face or leaks. Some masks are even designed to float on a cushion of air.
Still, other distinct options are available. One consists of nasal pillows, which typically are plastic inserts that look like headphone earbuds that are inserted in the nostrils. These are an excellent option if you struggle with claustrophobia or don’t like the mask leaving marks on your face. They may not be everyone’s comfort choice, however.
Some other masks are large enough to cover both the nose and mouth, which can compensate for those who mouth-breathe. This can prevent dry mouth. There are even masks that cover the entire face, including the eyes. Other mask interfaces act like a mouthpiece and can correct jaw positioning while delivering CPAP treatment.
2: Get Fitted With the Appropriate Size

Most people are fitted with a mask in the context of a sleep study, sometimes called a titration study. The purpose of this study is to introduce you to CPAP, present you with a few of the mask interface options, find the proper size, and allow you to try it out while the pressure setting is determined.
The staff who run sleep studies often have a favorite handful of masks that work well for most people. Chances are they will try these out on you first. Don’t be afraid to ask for other options, and, more importantly, don’t be afraid to ask for a different size. Whether at a sleep study, sleep clinic or at the durable medical equipment provider that is supplying your equipment, they should be willing to help you out.
Most mask interfaces come in a spectrum of sizes, and these depend on the manufacturer. There may be plastic sizing templates available. Some masks may have intermediate sizes such as “medium-small” and helpful accommodations like “wide.” Try to select a mask that is large enough to allow adequate air delivery. Avoid over-sized masks that may be prone to shifting on your face or excessive leaking.
Make certain to try it on while it's attached to a machine delivering your level of air pressure. Put on the headgear and get the full experience.
Try to replicate real-world use the best you can before you take it home and realize that when you lie on your side the thing leaks like a sieve, or when you strap it in place the pressure across the bridge of your nose is intolerable.
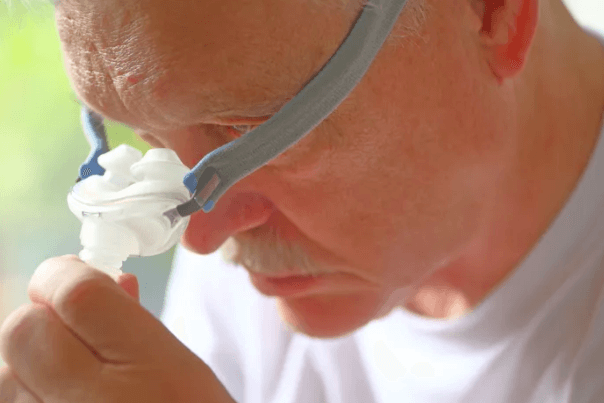
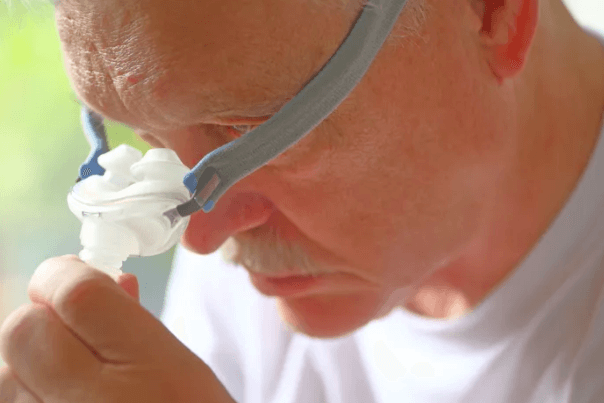
3: Use Accessories That Can Make Compliance Easier

Aside from getting the proper style and fit, you may also want to explore some of the other CPAP accessories that make treatment easier to tolerate.
The headgear that is used to secure the CPAP mask to your head can have as varied features as the mask interfaces. Many are made of fabric that is machine-washable. Some may have Velcro to customize the fit. Others may have plastic quick-release clips that allow you to fit it properly once, and then take it on and off easily. This way you don’t have to constantly adjust and readjust to find the perfect fit every time you use it.
If you are finding yourself breathing through your mouth, you may need to try a chinstrap.
Most people benefit from using a heated humidifier attached or built into the CPAP machine to moisten the air. There is also heated tubing that prevents moisture or condensation in the tubing.
If you have trouble tolerating the pressure as you fall asleep, you may want a machine that has a ramp function that starts at a low pressure and then builds up to your treatment pressure over a set period of time.
If the plastic bothers your skin, or if you are having trouble getting a good seal without excessive air leak, you may want to look into using a mask liner. There are also pads and cushions that can improve the fit of the mask.
There are many convenient options available to you, and these can make your life better and the chance of you complying with the treatment more likely.
4: If Things Are Not Working, Address Problems Earlyr
If you run into problems early or aren’t seeing a benefit, you are less likely to want to keep it up. Therefore, it’s important to address problems early or you may feel like giving up.
If your mask is the wrong size, if it leaks too much, if it leaves sores or marks on your face, or you have any of the numerous other problems associated with CPAP use, get help. You may need to talk to your equipment provider or your sleep doctor to get things fixed. Remember that you are a valued customer and they are running a business, so if they aren’t willing to help you out, find someone else who will.
Finally, keep your equipment clean by following the cleaning guidelines and replace things as they wear out. Most insurance policies will cover regular replacement of CPAP equipment, including masks, so look into how often you can update yours.
Why to Clean Your CPAP
First, take a moment to consider the importance of keeping the CPAP equipment clean. You're directly breathing the air that's circulated through the machine. The air is humidified and filtered, but it should be kept as clean as possible.
Cleaning can help to avoid potential dangers and problems, including the following:
• Bacteria exposure2
• Mold exposure
• Allergy symptoms
• Possible increased risk for sinus infections or pneumonia
• Musty or foul odor
• Mineralization within the equipment
• Premature equipment breakdown
• Voiding the device warranty
If cleaning is so important, how should it be done? Fortunately, it can be accomplished relatively easily at little expense.
How Often to Clean Your CPAP
Your equipment provider or sleep medicine physician may recommend routine cleaning of your equipment. Daily cleaning of the mask, tubing, and water chamber is often suggested by durable medical equipment suppliers and manufacturers.2 This may seem excessive. Fortunately, the risk of any sort of infection or mold exposure is extraordinarily low.
For optimal hygiene, it's recommended that the equipment be cleaned at least on a weekly basis.
If you are sick with an upper respiratory infection, you may want to clean up the equipment at this time. It is further recommended that you not share the equipment with others as this may cause an infection to be shared.
CPAP can be an effective treatment for obstructive sleep apnea, but it only does you good if you use it. If you struggle, speak with your sleep specialist or an APP-NEA network physician or dentist about other options i.e. Oral Appliance. It is always possible to be successful, but you may need some initial help.