Treatment for respiratory depression related to COVID-19 and Obstructive Sleep Apnea is the same – Oxygen. This is no coincidence. Oxygen is the catalyst, without which life would cease to exist. Oxygen plays a critical role in cellular respiration, the energy-producing engine that drives the metabolisms of all living beings.
Research has shown that those who experience the most severe COVID-19 symptoms are often obese. A recent published meta-analysis found that obese individuals who tested positive for COVID-19 were 113% more likely to be hospitalized, 74% more likely to be treated in ICU, and had a 48% higher rate of mortality than non-obese individuals. and in 2 small studies of individuals admitted to the ICU with confirmed COVID-19, researchers reported that OSA was present in 21.0% and 28.6 of patients, respectively.
Obstructive sleep apnea (OSA) is a common and serious disorder in which breathing repeatedly stops for 10 seconds or longer per event, hundreds of times during sleep. This disorder results in decreased oxygen in the blood and briefly awaken sleepers to start breathing again, repeatedly throughout the night. In adults, the most common cause of obstructive sleep apnea is excess weight and obesity, associated with excessive fat deposits in the soft tissues of the neck, below the tongue and throat. During sleep, when the throat and tongue muscles are more relaxed, this pressure caused by excessive fatty deposits, compress the soft tissues causing the upper airway in the throat to become blocked which results in restricted airflow into the lungs. In children, causes of obstructive sleep apnea often include enlarged tonsils or adenoids and dental conditions such as a narrow palate or excessive overbite but childhood obesity is also a major contributor to the development of obstructive sleep apnea as well, though it's much less commonly associated with the condition than adult obesity.
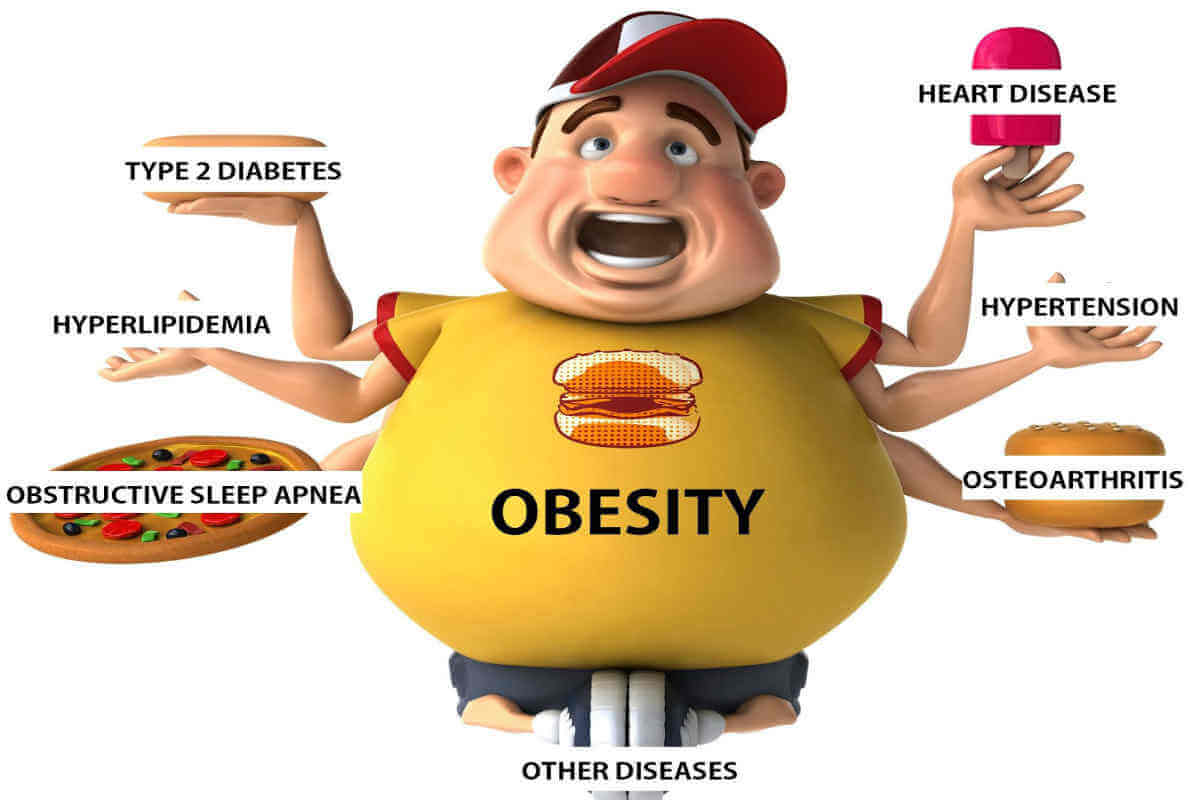
People with obesity are more likely than normal-weight people to have other diseases that are independent risk factors for severe COVID-19, including heart disease, lung disease, and diabetes. They are also prone to metabolic syndrome, in which blood sugar levels, fat levels, or both are unhealthy.
Weight gain is a major predictor of metabolic syndrome with waist circumference being a more sensitive indicator than body mass index as it reflects both abdominal subcutaneous adipose tissue and visceral adipose tissue. Visceral adipose tissue has more metabolic activity and secretes a number of hormones and pro?inflammatory cytokines which are linked with the metabolic abnormalities listed above. The biology of obesity includes impaired immunity, chronic inflammation, and peripheral blood that's prone to clot, all of which can worsen COVID-19.
The physical pathologies that render people with obesity vulnerable to severe COVID-19 begin with mechanics: Fat in the abdomen and chest pushes up on the diaphragm, causing that large muscle, which lies below the chest cavity, to impinge on the lungs and restrict airflow. This reduced lung volume leads to reduced airflow in the lower lobes of the lungs, where more blood arrives for oxygenation than in the upper lobes. This physical pathologic process known as obesity hypoventilation is also linked to worsening of OSA severity. Hypoventilation and OSA lead to decreased oxygen saturation. Oxygen is brought into the lungs and then passed into the blood across the alveolar membrane. During an obstruction of the airway or reduced airflow as in hypoventilation, the amount of oxygen bound to the red blood cells drops below a critical threshold and as a result the red blood cells start to lose their bound oxygen and begin to deform and coagulate causing clots in blood vessels in the lungs, heart and brain. Untreated OSA is the number 1 leading cause of pulmonary embolism, and heart attacks and strokes during sleep.
Other issues compound these mechanical problems. For starters, the blood of people with obesity has an increased tendency to clot—an especially grave risk during an infection that, when severe, independently peppers the small vessels of the lungs with clots and because COVID-19 injures endothelial cells, which respond to the insult by activating the coagulation system. Add obesity to the mix, and the clotting risk shoots up in COVID-19 patients with OSA.
It is likely that COVID-19 increases oxidative stress and inflammation and has effects on the bradykinin pathways, all of which are also affected in OSA patients. When you have these mechanisms already affected, it’s not surprising that COVID-19 affects them more strongly.
OSA patients with COVID-19 experience difficulty with their breathing and may notice that their CPAP pressure setting may not be enough to overcome their depressed respiratory effort. An increase in the CPAP pressure setting can cause more discomfort than otherwise experienced and the need to keep the machine cleaner than normally becomes an absolute must during this time as viral particles left in the machine can cause a reinfection which can be forced into the lungs making the patient critically ill. For those patients who are not compliant with their CPAP, it is an absolute must to consult with their medical provider and investigate the option of using a Dental Device called Mandibular Advancement Appliance which looks and feels like a mouth guard and gently and passively opens the airway by moving the lower jaw forward and allowing for improved breathing.
Conclusion: Being overweight or obese, increases the individual’s risk for OSA and developing COVID-19 related health complications, more than normal weight individuals. If an individual has been diagnosed with OSA and tested positive for COVID-19, even if asymptomatic, it is urgent that they seek immediate medical advice and make sure they are compliant with their treatment for OSA and if they are not compliant or can’t tolerate their CPAP, to get a referral for a tele-dental visit with a qualified dentist trained in dental sleep medicine to establish candidacy for an oral appliance.